An anterior pelvic tilt (APT) is one of the most common postural imbalances observed in clinical and movement settings. While a mild tilt is natural, excessive anterior tilt can contribute to lower back pain, hip dysfunction, core instability, and even shoulder or neck issues due to compensatory patterns.
Before creating a treatment or movement plan, it’s essential to evaluate the pelvis in context—looking at posture, mobility, muscle imbalances, and body awareness. In this article, we’ll explore what an anterior pelvic tilt is, how to recognize it, and how to assess it effectively in a therapy or movement setting.
🧠 What Is an Anterior Pelvic Tilt?
An anterior pelvic tilt occurs when the front of the pelvis drops forward and the back of the pelvis rises, increasing the curve (lordosis) in the lumbar spine. It’s often the result of a muscle imbalance involving:
- Tight/overactive: hip flexors (e.g., iliopsoas, rectus femoris), lumbar erectors
- Weak/inhibited: glutes, hamstrings, and deep core (especially transverse abdominis)
This postural pattern can lead to:
- Lower back tightness or pain
- Hip flexor strain
- Gluteal inhibition
- Altered gait or limited mobility
🔍 How to Evaluate an Anterior Pelvic Tilt
A full assessment includes visual analysis, palpation, functional movement testing, and awareness checks. Here’s a step-by-step guide.
✅ 1. Visual Postural Assessment (Standing)
Have the client stand in a relaxed, natural posture. Observe them from the side.
Look for:
- The ASIS (anterior superior iliac spine) noticeably lower than the PSIS (posterior superior iliac spine)
- An exaggerated lumbar curve (lordosis)
- Protruding abdomen or forward-tilted pelvis
- Glutes sticking out ("duck butt")
💡 Tip: Place your hands on the ASIS and PSIS and compare their vertical alignment—on a neutral pelvis, they should be roughly level.
✅ 2. Palpation & Bony Landmarks
Palpate the ASIS and PSIS to assess the tilt of the pelvis manually. You can also:
- Palpate hip flexors and quadratus lumborum for tightness
- Check glutes and hamstrings for tone and activation
- Assess abdominal tone or distension (a flared ribcage often accompanies APT)
✅ 3. Thomas Test (Hip Flexor Length Test)
Lay the client supine on a table, with one leg pulled to the chest and the other hanging off the edge.
Positive signs of APT:
- Hanging leg doesn’t drop parallel to the table → tight iliopsoas
- Knee doesn’t bend to 90° → tight rectus femoris
- External rotation of the leg → tight tensor fasciae latae or sartorius
✅ 4. Plumb Line or Grid Wall Observation
Use a plumb line or posture grid and have the client stand sideways.
Check if:
- The ASIS is anterior to the plumb line
- The lumbar curve is significantly deep
- The rib cage flares forward
✅ 5. Functional Movement Tests
Evaluate how the pelvis behaves during movement:
- Hip Hinge Test – Do they hinge from the hips or extend from the lumbar spine?
- Squat Assessment – Do they overarch the lower back or tip the pelvis forward at the bottom?
- Leg Lowering Test (Supine) – Do they lose spinal contact early, suggesting weak core control?
✅ 6. Core Engagement Check (Body Awareness)
Have the client lie supine with knees bent (hooklying position). Ask them to flatten the back against the floor.
- If they can’t posteriorly tilt the pelvis, this suggests poor core-glute engagement and dominance of hip flexors.
Ask them to find "neutral pelvis" and see how familiar or foreign the position feels—lack of awareness is common in APT clients.
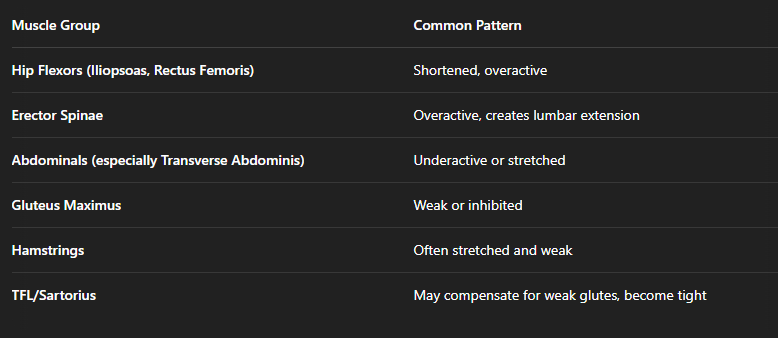
📍 Key Muscles to Watch in APT
🧘 Additional Observations
- Breathing patterns: Chest breathing and rib flare often accompany APT.
- Gait analysis: Overstriding or anterior pelvic rotation during walking/running.
- Core control: Difficulty activating deep core muscles without tilting pelvis forward.
🔚 Conclusion
Evaluating anterior pelvic tilt goes far beyond checking posture—it’s about understanding the body’s compensation patterns, muscle imbalances, and movement habits. By combining visual assessment, palpation, and functional testing, you can pinpoint the causes of APT and create a more targeted and effective treatment plan.
Helping clients become aware of their pelvic alignment is often the first step toward restoring balance—not just in the hips and spine, but throughout the entire kinetic chain.

